Hey there! If you’re struggling to make sense of eczema, you’re definitely not alone. From puzzling questions about what sets off those frustrating flare-ups to navigating the maze of treatment options, it can all feel a bit overwhelming.
That’s why we’ve gathered some of the most frequently asked questions about eczema. Think of this as your friendly guide to getting clear, helpful answers so you can better understand and manage your skin’s unique needs.
What is eczema, and how do I know if I have it?
Eczema isn’t just one thing; it’s actually a group of conditions that make your skin red, itchy, and inflamed. You might also hear it called dermatitis, which is a general term for skin inflammation.
If you’re experiencing symptoms like persistent itching, dryness, redness, or even rashes, you might be dealing with eczema. The way it looks and feels can vary a lot from person to person and even change over time. You might notice dry, scaly patches, or in more active phases, you could see redness, swelling, and even oozing or crusting.
For a deeper dive into what eczema involves, check out [What Is Eczema? (And What It Isn’t)].
Quick Note:
It’s important to know that eczema is typically a chronic condition, meaning it’s long-lasting. It often involves periods where symptoms are more intense (flare-ups) followed by periods of improvement. Remember too that these symptoms can appear differently depending on your skin tone. On lighter skin, eczema often looks red, while on darker skin, it might appear darker brown, purple, or ashen gray. We discuss how symptoms appear on various complexions in [How Eczema Looks on Different Skin Tones].
Quick Note:
If you’re concerned about your skin, the best first step is always to chat with a doctor. They can take a look, ask about your medical history, and help figure out if what you’re experiencing is eczema or something else. Learn more about the process in [How Doctors Diagnose Eczema (What to Expect)].
Is eczema contagious?
This is a really common concern, and the good news is: eczema is definitely not contagious. You can’t catch it from someone else, and you can’t spread it to other parts of your body just by touching or scratching.
Eczema isn’t caused by a virus, bacteria, or fungus. Instead, it’s largely due to a combination of genetics and how your immune system responds to things around you. We bust this common misconception in detail in [Is Eczema Contagious? Debunking a Common Myth].
What About Infections?
Sometimes, the broken skin barrier caused by eczema can become infected with bacteria or viruses, like staphylococcus aureus or the herpes simplex virus (which causes eczema herpeticum). While these secondary infections can sometimes spread, the underlying eczema itself is not contagious.
If you notice signs of infection, like pus-filled bumps, yellow crusting, or rapidly worsening skin, it’s important to see a doctor right away. But you can feel comfortable interacting with friends and family without worrying about passing eczema on.
What causes eczema?
There isn’t one single cause of eczema; it’s usually a complex mix of factors.
- Your genes play a significant role – eczema often runs in families. Learn more in ’16- The Role of Genetics in Eczema (And Why It Runs in Families)’.
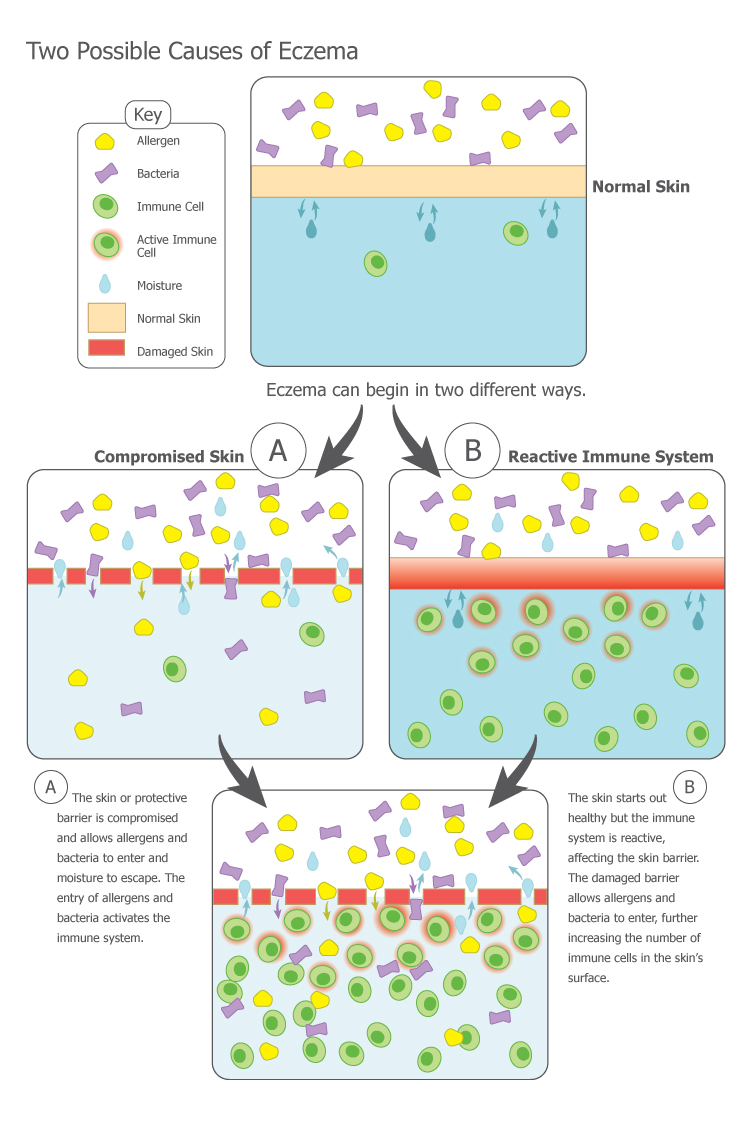
- People with eczema often have a defect in their skin barrier, the outer layer that protects us. This weakened barrier lets irritants and allergens in and allows moisture to escape, leading to dryness.
- Your immune system also plays a role, especially in atopic dermatitis, where it can overreact to triggers, causing inflammation.
- Then there are environmental factors – things like soaps, detergents, certain fabrics, extreme temperatures, and even stress can trigger or worsen eczema flare-ups.
For a more scientific look at the causes, see [What Causes Eczema? A Scientific Overview]. To understand what’s happening under the skin, read [How Eczema Works: Immune System, Barrier Function, and Inflammation].
Ongoing Research
Researchers are constantly learning more about the specific genetic and immune pathways involved in eczema. Understanding these mechanisms is key to developing new and more targeted treatments. Identifying your personal triggers is a big step in managing your eczema. You can learn more about common ones in [Contact Dermatitis: Top 10 Triggers], [Atopic Dermatitis: Top 10 Triggers], and [Understanding Trigger Categories: Irritants, Allergens, and More].
Are there different types of eczema?
Yes, absolutely! Eczema is an umbrella term for several distinct types of dermatitis. Knowing the type helps tailor treatment. Some common ones include:
- Atopic Dermatitis: The most common type, often starting in childhood and linked with allergies/asthma. See [What Is Atopic Dermatitis? (And How It Progresses Over Time)].
- Contact Dermatitis: A reaction to something your skin touches (irritant or allergen). See [What Is Contact Dermatitis? (With Real-World Examples)].
- Dyshidrotic Eczema: Causes tiny blisters on hands and feet.
- Nummular Dermatitis (Discoid Eczema): Shows up as coin-shaped itchy spots.
- Seborrheic Dermatitis: Affects oily areas like the scalp (dandruff), face, and chest.
- Stasis Dermatitis: Occurs on lower legs due to poor blood flow.
- Neurodermatitis (Lichen Simplex Chronicus): Thickened, leathery skin from repeated scratching.
We provide a comprehensive overview in [Our Guide to the Different Types of Dermatitis].
Why Knowing the Type Matters
Knowing which type of eczema you have is important because it influences your treatment plan and helps identify triggers. For instance, with contact dermatitis, figuring out the trigger is crucial. Patch testing can help identify allergens. If you need this test, [Patch Testing 101: What It Is, Who Needs It, and What to Expect] explains what’s involved. If you’re unsure about your type, a dermatologist can help.
How do I treat eczema?
There’s no one-size-fits-all answer, as treatment depends on the type, severity, and your individual needs. The main goals are to relieve itching and inflammation, heal the skin, and prevent future flare-ups. Common approaches include:
- Moisturizers (Emollients): Cornerstone of care. Use daily to hydrate and repair the skin barrier.
- Topical Corticosteroids: Prescription creams/ointments to reduce inflammation and itch during flares.
- Topical Calcineurin Inhibitors (TCIs): Prescription non-steroid topicals for inflammation, often used on sensitive areas.
- Topical PDE4 Inhibitors: Newer prescription topicals that also reduce inflammation.
- Oral Medications: For severe cases, pills like corticosteroids or other systemic drugs may be needed.
- Biologics: Injectable medications targeting specific immune pathways.
- Phototherapy (Light Therapy): Medically supervised UV light exposure to reduce inflammation.
For more details on common prescriptions, see [Most Common Medications Prescribed for Dermatitis]. Curious about non-prescription options? Check out [Natural Remedies and Alternative Therapies for Eczema: What Works and What Doesn’t]. Wondering about the doctor’s visit itself? Read [What Happens When You Visit the Doctor for Eczema?].
A Note on Topical Steroids:
It’s really important to use topical medications exactly as directed by your doctor. There’s sometimes fear or misinformation online about topical steroids (“corticophobia”). However, when used appropriately under medical guidance, they are safe and effective for managing flares. If you have concerns about any treatment, always discuss them with your healthcare provider. Beyond medications, identifying triggers, gentle skin care, and managing stress are also key.
How can I stop eczema from itching?
Oh, that relentless itch! It’s one of the toughest parts of eczema. Here are strategies that can help:
- Moisturize frequently: Keep skin hydrated to reduce dryness and the urge to scratch. Use a thick, fragrance-free moisturizer often, especially after bathing.
- Use cool compresses: Applying a cool, damp cloth can be soothing.
- Take lukewarm baths or showers: Hot water dries skin out. Keep bathing short, use mild cleansers, pat dry gently, and moisturize right away.
- Avoid scratching: Easier said than done, but scratching damages the skin barrier. Try gently patting or tapping instead. Keep nails short and smooth.
- Wear soft, loose-fitting clothing: Avoid rough or tight fabrics. Cotton is often a good choice.
- Manage stress: Stress can trigger flares. Healthy coping mechanisms like exercise or mindfulness can help.
- Talk to your doctor about medications: Antihistamines might help nighttime itching, and prescription topicals/orals target the underlying inflammation.
Itching often disrupts sleep; find tips in [The Connection Between Sleep and Eczema (Tips for Better Sleep)].
Side note:
The itch pathway in eczema is complex. Scientists are actively researching new treatments that specifically target the nerve signals causing that maddening sensation. Finding what works best for your itch might take some trial and error.
Can diet affect eczema?
For some people, particularly those with atopic dermatitis, food allergies can sometimes trigger or worsen eczema symptoms. Common culprits include milk, eggs, peanuts, tree nuts, soy, wheat, and fish. However, this isn’t the case for everyone with eczema.
Food can be one of many triggers explored in [Understanding Trigger Categories: Irritants, Allergens, and More].
Important note:
It’s crucial not to make drastic dietary changes without consulting with your doctor or an allergist. They can help determine if food allergies play a role (perhaps through testing) and guide safe elimination diets if needed. Eliminating foods unnecessarily can lead to nutritional deficiencies, especially in children. While diet isn’t the primary cause, paying attention to potential food triggers can be part of your management plan.
Can eczema be cured?
Currently, there is no known cure for eczema. It’s a chronic condition that many people manage throughout their lives.
However, the good news is that with the right treatments and management strategies, many individuals with eczema can achieve significant relief from their symptoms and enjoy a good quality of life.
Hope Through Research:
Research is constantly evolving, leading to a better understanding of eczema and the development of new, more effective treatments. The outlook for people living with eczema is continually improving. Think of managing eczema like managing other chronic conditions – it’s about controlling symptoms and living comfortably.
What should I do if I get an infection on my eczema?
Because eczema disrupts the skin barrier, it makes skin more vulnerable to infections. If you suspect an infection, it’s important to seek medical attention promptly. Signs can include:
- Sudden worsening of your eczema
- Oozing that’s thick, yellow, or pus-like
- Crusting or small, fluid-filled bumps (pustules)
- Increased pain or tenderness
- Fever (in some cases)
Your doctor can diagnose the infection and prescribe treatment (like antibiotics or antivirals). Treating infections quickly is key.
Recognizing Eczema Herpeticum
Be aware of eczema herpeticum, a specific viral infection (herpes simplex) that can be serious, especially for young children. It often looks like rapidly spreading, painful blisters or punched-out sores. If you suspect this, seek medical care immediately.
How does eczema affect my quality of life?
The impact of eczema goes far beyond just the physical symptoms. The constant itching, visible rashes, and sleep disturbances can significantly affect emotional well-being, social interactions, and overall quality of life.
Many people with eczema experience anxiety, depression, or frustration. It can impact relationships, work/school, and daily activities. We explore this aspect further in [The Emotional Toll of Eczema: Anxiety, Depression, and Coping].
Important note:
The connection between eczema and mental health is significant. It’s important to acknowledge this toll. If you’re struggling emotionally, don’t hesitate to talk to your doctor or seek support from a mental health professional or support groups. You’re not alone.
How can I manage eczema during the winter?
Winter can be tough for eczema due to cold, dry air and indoor heating. Tips include:
- Moisturize even more frequently.
- Use a humidifier indoors.
- Avoid hot baths and showers; stick to lukewarm.
- Dress in layers with soft fabrics next to the skin.
- Protect skin with gloves/scarves outdoors.
- Be mindful of drying activities (chlorinated pools, fireplaces) and moisturize after.
A Note for Older Adults:
The increased dryness and itchiness sometimes seen in older adults (“seventh age itch”) can be worse in winter. Consistent moisturizing is key.
What should I do if my child has eczema?
It’s tough seeing your child struggle. Key tips include:
- Establish a regular bathing and moisturizing routine.
- Identify and avoid triggers (soaps, fabrics, potential food allergens).
- Prevent scratching (short nails, cotton gloves at night, distraction).
- Follow your doctor’s treatment plan carefully.
- Educate your child about their skin as they grow.
- Offer emotional support and understanding.
For a comprehensive guide dedicated to this topic, please see [Eczema in Children: What Parents Should Know]. Since atopic dermatitis often starts in childhood, you might also find [What Is Atopic Dermatitis? (And How It Progresses Over Time)] helpful.
Side note:
Many children see improvement as they age, though some continue to have eczema into adulthood. Focus on effective management at each stage. Help is available from healthcare professionals and support resources.
Can stress make eczema worse?
Yes, absolutely. The stress and eczema connection is well-documented. While stress doesn’t cause eczema, it can definitely trigger flare-ups or worsen existing symptoms. Stress releases chemicals that increase inflammation, leading to more itchiness and redness.
We delve deeper into this connection and offer coping strategies in [Can Stress Trigger Eczema? (And How to Break the Cycle)].
Breaking the Cycle
It can become a frustrating cycle: eczema causes stress, and stress worsens eczema. Finding healthy ways to manage stress (exercise, mindfulness, hobbies) is an important part of breaking this cycle.
How do I know if I need to see a dermatologist for eczema?
Your primary care physician (PCP) can often manage mild/moderate eczema, but seeing a dermatologist (skin specialist) is recommended if:
- Your eczema is severe or not responding well to PCP treatments.
- Symptoms are significantly impacting your quality of life.
- You have frequent or persistent flare-ups.
- You’re not sure about your diagnosis or the type of eczema.
- You’re considering advanced treatments (phototherapy, biologics).
- Your child has severe eczema.
Learn more about the diagnostic process in [How Doctors Diagnose Eczema (What to Expect)]. For what happens during a visit, see [What Happens When You Visit the Doctor for Eczema?].
The Specialist’s Role:
Dermatologists have specialized expertise in complex skin conditions like eczema and can offer a wider range of diagnostic tools and treatments. Don’t hesitate to ask your PCP for a referral if needed.
Yes, particularly atopic dermatitis, is often linked to other allergic conditions like hay fever, asthma, and food allergies (sometimes called the “atopic march”). These conditions involve an overactive immune system reacting to harmless substances.
Explore this question further in [Is Eczema an Allergy, a Disease, or a Skin Condition?]. Allergens are one type of trigger discussed in [Understanding Trigger Categories: Irritants, Allergens, and More].
Clarifying the Connection:
While allergies can trigger eczema flares in some people, eczema itself is not simply an allergic reaction. It’s a complex condition involving genetics, skin barrier issues, and immune responses, where allergies are just one potential trigger. Allergy testing may help identify specific triggers if suspected.
Understanding the ins and outs of eczema – from what it is and isn’t to common triggers and treatments – can make a real difference in how you manage your condition. Getting answers to these FAQs is a great step toward feeling more informed and empowered.
Remember, you are not alone, and many resources and healthcare professionals are ready to support you.
Want to dive deeper into how eczema affects your daily life? Check out our article [How Eczema Affects Daily Life and Social Interactions] for helpful tips on navigating social and emotional challenges.